I come from a small village, “Konyango,” in the Western Part of Kenya (Kisumu County) along the Lake Victoria region where HIV is one of the most significant pandemics. Kisumu has the highest HIV prevalence, significantly above Kenya’s national average, with studies indicating a prevalence of around 17.5 per cent. With socio-cultural factors including poverty, lack of education and social dynamics of “Jaboya tradition” (sex in exchange for fish), new HIV infections continue to skyrocket in my hometown, particularly affecting women and adolescents. Growing up, the shadow of HIV/Aids was not a distant news story; it was a devastating reality that ripped through my family. I witnessed the slow and agonising decrease of loved ones – victims of a virus that seemed to steal not just life but the very essence of joy from my family and others.
The current state of HIV/Aids globally is worrying. While the US administration’s decision to stop foreign aid might have seemed progressive politically, developmentally, it halted life-saving systems, rendering many in the global south vulnerable and exposed to preventable deaths. In Kenya, the halt has disrupted HIV treatment and care. Kenya faces an ARV stock out, including second-line ARVs critical for developing resistance to first-line therapy, putting thousands of patients at risk. The shortage, which continues to leave thousands exposed, is also threatening to reverse progress made in realising the 95-95-95 global goal on HIV.
According to the World Health Organisation report, Kenya is among eight countries that could potentially exhaust the HIV treatment supply in the coming months. It, therefore, means increased HIV infections and Aids-related deaths.
Follow The Standard
channel
on WhatsApp
In the current digital age, the hope of realising the 2030 Sustainable Development Goals, especially Goal 3: Good Health and Well-being, is possible yet uncertain. A goal that aims to ensure healthy lives and promote well-being focuses on ending preventable deaths, ending epidemics like Aids and achieving universal health care is under threat. While intensive research and work is going on in finding an HIV vaccine, including the already developed and distributed HIV prevention technologies, the decrease in funding is deadly.
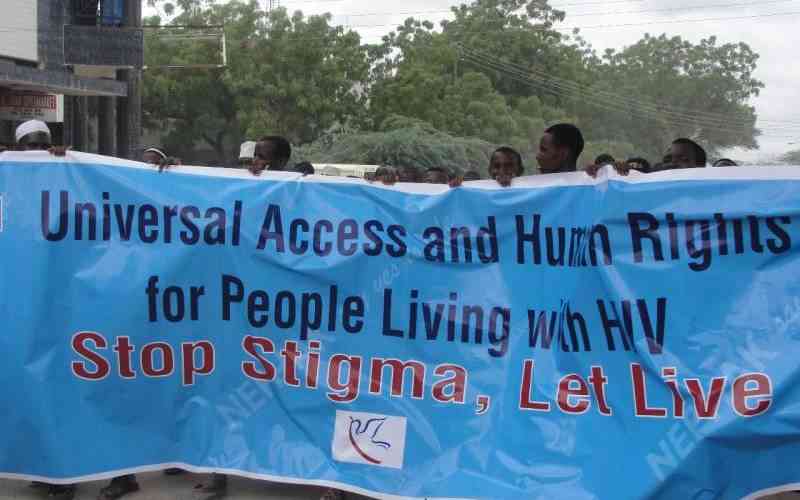
Moreover, we must understand the “intercases” of HIV/Aids. Its complex, intertwined realities of people living with HIV and dying from Aids aren’t to be fence-watched. Because it’s not just about the virus itself but the web of consequences: The crushing weight of deaths, the opportunistic diseases, and the profound, enduring grief loved ones are left with. As the globe yearns for a cure, a preventative measure, we need to creatively think of funding that can accommodate all three HIV implementation goals, prevention, care and treatment.
Governments need to intensify health care funding. Domestic resource mobilisation is essential and the first line of defence. Governments must increase budget allocation to health services while engaging local philanthropists and corporate social responsibility programmes. Additionally, communities need to be encouraged to invest in their human resources. Many times, volunteer opportunities aren’t quantified financially. However, these are intangible resources that contribute to overall health improvement through community education and awareness.
With the increasing digitisation, civil society organisations can explore crowdfunding avenues for public health interventions. Sourcing funding from the public ensures ownership and accountability. Furthermore, Africa can explore regional funding pools as the continent is most severely affected by the funding health crisis. The African Union, the African CDC, and other stakeholders can resource-mobilise funding for healthcare.
The financing can, therefore, be distributed to countries’ healthcare systems for improvement after a critical assessment of the health risks, opportunities, gaps, and challenges. However, there needs to be a precise accountability mechanism that ensures health funding isn’t misappropriated and that penalties, such as percentages of the amount paid back, are included in policies.
Follow The Standard
channel
on WhatsApp
By Evelyn Odhiambo